Cambs LMC Committee Election – Nominations Open!
Are you a Partner, Sessional, or Locum GP, on the Medical Performers’ list in Cambs & Peterborough?
Do you feel passionately about advocating on behalf of, and protecting local general practice?
Would you like to be part of the statutory representative voice for Cambs & Peterborough GPs?
Would you like to be one step ahead with key local & national issues among a dynamic committee?
Could you help shape the future of Cambridgeshire & Peterborough general practice?
If you’ve answered YES to the above, then you should nominate yourself to stand for election to join the Cambs LMC Committee – the collective professional voice of Cambridgeshire & Peterborough General Practice, funded by GPs, for GPs.
Cambs LMC is the organisation that supports, represents, and advises all GPs across the county, regardless of contractual status. There are 24 committee members and 3 registrars who are supported by a fantastic executive team.
We confidentially discuss a wide range of topics affecting both local and national general practice. Currently, we have excellent representation from partners, sessional, and locum GPs, which we want to continue. The committee is especially welcoming, describing themselves as the LMC family, we are supportive of each other and nurture the new members with a fellow committee member mentor.
Above all, we value the safe space we create to hear and respect each other’s views. It is vitally important that Cambs LMC remains representative of general practice across the county.
GP Collection Action – Secondary Care Guidance
Thank you all for continuing to develop and expand on our collective action to protect our patients and practices.
We recognise the particular challenges across the primary and secondary interface, and want to ensure all specialist colleagues are aware of the purpose and aims of GP Collective Action. To this end GPC England and the UK Consultants Committee have developed explanatory resources hospital and trust-based colleagues.
Our new webpage https://www.bma.org.uk/secondarycareGPaction outlines how secondary care colleagues may be affected and ways they can support GPs in this campaign. This includes a downloadable PowerPoint presentation which LNCs (Local Negotiating Committees) can use in their patch, an at-a-glance fact sheet that can be displayed in Trusts, and a recorded webinar offering further insights.
Please also continue to refer to our collective action Protect your patients, protect your practice webpage, which explains in more detail the nine actions that practices can choose to take. It also contains more information such as the Safe Working Guidance Handbook, Campaign resources and Patient materials.
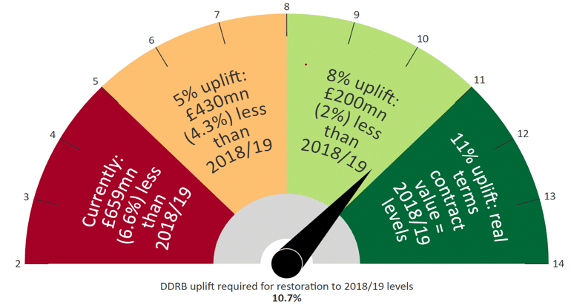
As negotiations for the GP contract 2025/26 progress, this is a pivotal moment for all GPs to unite as a profession – not just for safe and sustainable general practice, but for a safe, sustainable and stronger NHS too.
Primary Care Joint Parliamentary Event – 28 January
GPC England jointly hosted an MP parliamentary drop in event for MPs in Westminster. The event on the future of primary care was held jointly with the British Dental Association, Community Pharmacy England, the Optometric Fees Negotiating Committee and the Association for Primary Care Audiology Providers and was attended by over 40 MPs. These included members of the health and social care select committee and shadow health ministers. During the event we outlined key concerns related to workforce and funding and encouraged MPs to sign a joint letter to the Health Secretary calling for increased support for primary care.
NHS Mandate and NHSE Planning Guidance – improving access to General Practice
Published last week, the UK Government’s new mandate for the NHS and NHS England’s planning guidance for 2025/26 both emphasise improving patient access to general practice and primary care. Neither document establishes clarity in terms of how this will be achieved, but the new Mandate does refer to investment in upgraded GP surgeries and in data and digital tools.
2023-24 Type 2 Pension Forms for Sessional GPs
We have recently highlighted the change of form and upload process for type 2 pension forms for 2023-24. Sessional GPs are required to complete a Type 2 Self-Assessment for each pension year, so that NHS England can ensure that all NHS pension contributions have been correctly paid and then accurately allocated to that GP’s NHS Pension Scheme record.
The relevant forms must be completed by those who have undertaken practitioner pensionable work between 1 April 2023 and 31 March 2024, and should be submitted to PCSE by 28 February 2025. PCSE and the BMA Pensions Committee have held two webinars to explain the new form and the process to upload the forms. Watch a recording of the webinar
Resident Doctor dispute on exception reporting
Despite its best-efforts during negotiations, the BMA’s UKRDC (UK resident doctors committee) have announced they will be entering into a dispute with the Government over the contractual reform of exception reporting (ER). The GPRC (GP registrars committee) met last week and passed a motion which offers their full support to UKRDC in entering a dispute to drive the negotiations to an effective resolution. Read more here
GPC England Regional Elections – coming soon
GPs Committee England will soon be seeking nominations for voting members of the committee for the 2024-2027 sessions, we will be electing one representative from each of the following regions:
- Cambridgeshire and Bedfordshire
- Hertfordshire
- North and South Essex
- Barking & Havering, Redbridge & Waltham Forest and City & Hackney
- Cumbria and Lancashire
- Wigan & Bolton, Bury & Rochdale and West Pennine
- South & West Devon and Kernow
- Hampshire and Isle of Wight
- Kent
- Surrey and Croydon
- East Yorkshire, North Lincolnshire and Lincolnshire
- Calderdale, Kirklees, Leeds and Wakefield
For more information about BMA elections