Rebuild GP Campaign – The Fight Against GP Bureaucracy
Our colleagues at Rebuild GP are launching a new campaign: we need to let Government, NHS England and our patients know about the massive and unsustainable amount of unnecessary paperwork, admin and red tape we have to tackle daily in order to care for our patients.
The link to the website can be found here: https://rebuildgp.co.uk/the-fight-against-gp-bureaucracy
It includes shareable content for social media, contacts for campaigning, and shareable graphics for your surgery wall/website.
- GPs are not short of effort. We are short of time.
- Every unnecessary task pushed into general practice means fewer appointments for patients.
- You cannot fix access while loading more admin onto GPs.
- Take bureaucracy off our desks and put patients first.
- Patients are frustrated. GPs are exhausted.
- The common problem is bureaucracy stealing time from care.
- This has to change.
As always, please keep in touch with us at the Cambs LMC office with any questions, examples, and feedback.
National Updates from BMA
General Practice: Critically Endangered – Facing Extinction
Many thanks to those of you who logged in to the recent webinars. It was great to connect with over a thousand GPs joining and contributing to where we are now, and the future direction of travel ahead of coming back to you with more information next month regarding the 2026/27 contract. BMA expects to receive the final position from government at the end of the month. GPC England will also then meet, scrutinise and vote thereafter, and will start webinars on the new contract – and your opportunity to feed back on it – at the start of March.
For those of you unable to join, BMA will be publishing a shortened 30-minute podcast and will also be sharing ‘bite size’ briefings on what we need to see from NHS England to fill the vacuum of ‘Neighbourhoods’ as well as expanding on the themes we covered around our profession being critically endangered, and facing extinction:
The loss of our habitat through starvation of premises funding; over-exploitation via being expected to absorb rising demand; greater clinical complexity; workload shifts and greater bureaucracy, compliance and regulation all with fewer GP:Patient ratios is classic over-harvesting. Our pollution isn’t chemical – it’s cognitive overload: paperwork, box-ticking, regulation, red tape and IT friction leading to productivity and morale collapse. GP substitution grows with new roles with no boundaries and unlimited supervision; destabilising the GP eco-system instead of strengthening it. And climate change – the constant policy churn, the drives on access and media pressure allowing no time for our species to adapt before the next reorganisation lands.
BMA will be expanding on this in light of the new contract next month. We know how vital these discussions are to the whole profession, BMA wants your feedback and to bring you along, so please feed in any queries you have to info.gpc@bma.org.uk
Dates and links to register for the March 2026/27 contract webinars will follow in the next newsletter.
Focus on: Vaccination by non-registered healthcare workers
GPC England has published a ‘Focus on guidance on vaccinations by non-registered healthcare workers, following an update by the UK Health Security Agency (UKHSA) to their guidance on the national minimum standards and core curriculum for vaccination training.
UKHA’s guidance outlines the requirements for vaccinating staff, including the role non-registered healthcare professionals should play in the provision of vaccinations. This clarification around the role of HCSWs may not be in line with existing interpretation and could potentially significantly impact upon the way in which practices design and deliver mass vaccinations programmes.
Read the GPC England guidance: Vaccination and immunisation programmes
Letter to CMO about vaccination programmes
BMA has written to the Chief Medical Officer, Professor Chris Whitty, to highlight concerns about lack of funding uplifts for GP practices providing routine and seasonal vaccination programmes. Despite an agreement from NHS England to uplift the payments for routine childhood vaccinations by £2 per dose, funding for GP vaccination programmes has fallen significantly behind inflation during this time, losing over a quarter of its value. Safeguarding and increasing uptake for these programmes should be a priority for the Government and the NHS, especially in light of the risks we’ve seen in recent years from infectious diseases alongside falling rates of vaccination. BMA will continue to pursue all avenues, to support practices.
NHS England Chaperones & Prevention of Sexual Misconduct in the NHS Guidance
BMA are writing to NHS England further to the publication of their document Improving chaperoning practice in the NHS: key principles and guidance following its publication in December. This guidance, and its implementation, form a key part of the actions listed in the Update on actions to prevent sexual misconduct in the NHS released on the same day.
GPs and their practices treat the protection of patients and staff alike with the utmost seriousness, and whilst we support the principles behind this guidance and recognise the potential for staff isolation, the fact that so many consultations are one-on-one presents issues for practices regarding keeping all who use, and work in, the service safe.
ICBs will be expected to provide support for practices in implementing these new standards, but some aspects of the guidance will be challenging to implement fully, with the chaperoning guidance in particular presenting practical difficulties as the document represents a significant expansion of the typical practice policy. BMA would highlight the following:
- Chaperones for all intimate examinations in patients under 18 (this would mean a GP carrying out a new baby check, or assessing nappy rash would need a chaperone for example, and this would need to be separate to the parent or family member bringing the child)
- Chaperones for online and telephone appointments (it’s difficult to see how this can be practicably offered)
- Home visits (the guidance recognises the challenges of lone working, but does not acknowledge the capacity constraints, nor the impact of small practice sizes as factors)
GPC England will be reflecting on the need for proportionality, common sense and patient/parent choice to reassure GPs and their teams, and will continue to keep you updated.
Joint primary care parliamentary reception
BMA jointly held a parliamentary drop-in reception, alongside other organisations for MPs and their staff on the crisis in primary care. Over 20 MPs attended the event, hosted by Liberal Democrat Primary Care Spokesperson Helen Maguire MP, including the Shadow Primary Care Minister, Luke Evans, Dr Simon Opher MP, Ian Sollom, Lee Pitcher, Dawn Butler and Pippa Heylings.
BMA briefed attending MPs about the current crisis in general practice particularly focussing on finance and GP under and unemployment, and spoke about concerns regarding neighbourhood models and the Carr-Hill formula review. Over the coming weeks BMA will continue to brief MPs from across all parties on these issues and its asks to resolve the current crisis and ensure general practice is supported to meet the needs of patients now and in the future.
Practice Finance research: results and call to action
BMA would like to thank everyone who took the time to share practice accounts data via the recent survey and have now analysed the initial results. Key insights have been shared with NHSE and the DHSC, ensuring their awareness of the financial pressures facing GP practices in England.
You can see the key insights for yourself here.
But it’s not too late to help with this research. The survey remains open on a rolling basis, so BMA can build a growing and increasingly robust resource that will be of immense importance during the new substantive GP contract negotiations.
- Did you start inputting data but were unable to complete your submission? Not to worry – incomplete responses have been saved. You can access them via a link that has been sent to your email address. Alternatively, head here and click on ‘Already started? Pick up where you left off’.
- Do the results not chime with what you’re seeing at your practice? Help us make the insights more accurate by sharing your data now. Only anonymised data will be shared with the BMA, and only anonymised and aggregated data will be shared any further.
- Did you already complete the survey? BMA is immensely grateful. If you can, keep up the good work and enter your accounts data for the next financial year (2025/26) once you can.
Professional obligations and protecting patients first and foremost
Some LMCs have reported concerns from GP partners who have received contract breach notices from ICBs in circumstances where practices believe their actions were taken to comply with professional duties under Good Medical Practice (GMP).
GPC England is seeking examples to better understand the nature, frequency and consequences of these situations. In particular, we are keen to hear from GP partners where alleged breaches arose from decisions made to protect patient safety, maintain professional standards, or act ethically in line with General Medical Council expectations – for example in relation to workload pressures, safe staffing, continuity of care, or limits on capacity.
GPs are legally and professionally required to practise in accordance with GMP, putting patient safety, dignity and quality of care first. Where contractual requirements or commissioning expectations appear to conflict with those professional obligations, practices may feel they have little choice but to act in the interests of patients, even where this risks challenge from commissioners.
Understanding how ICBs are interpreting contracts, and how breach processes are being applied in these circumstances, is essential to informing GPC England’s national policy work, supporting LMCs locally, and strengthening our collective position in discussions with NHS England and DHSC.
If your practice has received a breach notice that you believe relates directly to actions taken to comply with GMP, BMA would welcome a brief outline of the situation. This may include the nature of the alleged breach, the professional considerations involved, and any outcomes to date. Examples can be shared confidentially and anonymised as necessary.
Please share details with your LMC or with GPCE via info.gpc@bma.org.uk. Your experiences are vital in ensuring GPs can uphold their professional responsibilities without fear of inappropriate contractual sanction.
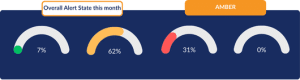
GP pressures – workforce and appointment data
The latest GP workforce data showed that in December 2025, the NHS had the equivalent of 28,777 fully qualified full-time GPs. While there is a general rise in FTE GPs since July 2023, GP practices still employ the equivalent of 587 fewer FTE GPs than in September 2015. In addition, the number of GP practices in England has decreased by 7 over the past year to 6,174.
This fall in both GP numbers and practices coincides with a rise in patients: as of December 2025, there was 63.9 million patients registered with practices in England with each FTE GP responsible for an average of 2,220 patients. This is an increase of 282 patients per GP, or about 14.6%, since 2015.
Despite this, 30.9 million standard appointments were delivered in December 2025 – an average of 1.47m appointments per working day, higher than Dec 2024 (1.41m) and Dec 2023 (1.36m).
Read more about GP pressures on the data analysis page, which shows the level of strain GP practices in England are under: Pressures in general practice data analysis
How to get the most out of the LMC Support Network
- Join the LMCSN WhatsApp group– an opportunity to share questions/thoughts/peer support.
- Use the web forum for discussions, this will enable you to go back and catch up on conversations in an easy-to-follow way.
- Share service level agreements for locally commissioned services to build up a comprehensive library and list fees by service for ease of reference. This can help in future local negotiations.
- Share any documents/templates/posters/videos so that they can be hosted on the website allowing the greater LMC family to use and be inspired to do similar.
- Come to virtual monthly LMCSN meetings which is an opportunity to share questions / thoughts / peer support as well as hear from and ask questions to the GPC England colleagues.
To share materials or ideas/comments etc, please email admin@lmcsn.co.uk
If you want to access the website/forum/WhatsApp, join here https://lmcsn.co.uk/join-us
Find out more at the WhatsApp community and website at www.lmcsn.co.uk